Complete Otosclerosis ENT 2013, 2016, 2019
Otosclerosis is a condition where one or more foci of irregularly laid spongy bone replace part of normally dense enchondral layer of bony otic capsule in the bony labyrinth. This is one of the most common question in DNB ENT THeory and OSCE,We will start with anatomy and then go for clinical findings and treatment options.
Questions on Otosclerosis – Discuss in brief the aetiopathogenesis of otosclerosis. Describe in brief the management of otosclerosis with special reference to “Revision Surgery”.Q-Clinical features and audiological eligibility for surgery. Define Otospongiosis, its clinical features, surgical treatment and its complications. Q- a) Describe histopathology & genetic basis for Otosclerosis. Clinical, audiological & radiological diagnosis of Otosclerosis. Surgical challenges in Stapes surgery. Describe the various options to make fenestra during stapes surgery and various prostheses being used with the method of placement. (4+4+2) Dec 2013, Dec 2016, Dec 2018, Dec 2019, June 2019
Anatomy of labyrinth.
- Otic capsule
- Otic labyrinth
- Periotic labyrinth
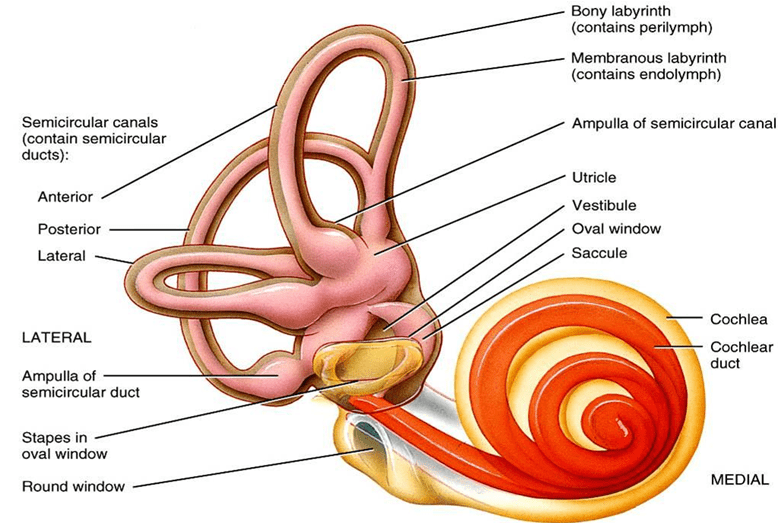
Otic Capsule
- It is the bony labyrinth
- Ossifies from 14 centres
- First one > region of cochlea >16 weeks
- Last one > posterolateral part of posterior semicircular canal > 20 weeks
- It has three layers:
- Endosteal
- Enchondral
- Periosteal
- Endosteal layer : Innermost layer.It lines the bony labyrinth
- Enchondral layer : Develops from cartilage and later ossifies into bone(ENCHONDRAL LAYER :some islands of cartilage left unossified & give rise to otosclerosis).
- Periosteal : Covers the bony labyrinth
- Periotic / Peilymphatic Labylinth : It surrounds the otic labyrinth and is filled with perilymph. It includes vestibule,scala tympani,scala vestibuli,perilymphaticr space of semicircular canals and the periotic duct.

Epidemiology :
- 10% overall prevalence of histologic otosclerosis
- 1% overall prevalence of clinical otosclerosis
- Race(% incidence of otosclerosis)
- Caucasian(10%)
- Asian(5%)
- African american(1%)
- Gender
- More common in females than males in the ratio 2:1
- Age
- Most common age of presentation : 15-45yrs
- Youngest presentation : 7yrs
- Oldest presentation : 50yrs
Pathogenesis of Otosclerosis
- Resorption of enchondral bone
- Enlarges perivascular space
- Deposition of immature woven bone
- Further remodelling
- Deposition of mature sclerotic bone
- Bone remodelling controlled by osteoblasts and osteoclasts
- Growth factors,cytokines,enzymes and free radicals
- Failure of regulation of osteoclasts and osteoblasts
- Uncontrolled bone remodelling
Phases of Otosclerosis
- Two phases of disease:
- Active/Immature/Otospongiosis phase
- Inactive/Mature/Otosclerotic phase
Active Phase :
- Deposition of immature woven bone
- Increased cellularity
- High vascularity
- Dilatation of vessels
- Schwartz sign
Blue Mantles of Manasse :

Mature Phase :
- Deposition of highly mineralised bone
- Mature bone-thick and cellular
- Osteoclastic activity resolved
- Vascular spaces narrowed
Most common sites of involvement:
- Fissula ante fenestrum- 80-95%
- Round window niche- 30%
- Apical medial wall of cochlear labyrinth- 15%
- Stapes footplate- 12%
- Posterior to oval window
- Anterior wall of IAC,cochlear aqueduct,malleus,incus
Types :
1: Histological
- Stapes not involved
- Diagnosed by postmortem examination of temporal bone
2: Stapedial
- Stapes involved
- Conductive hearing loss
3: Cochlear
- No stapes fixation
- Involves cochlear endosteum
- Sensorineural hearing loss
Etiology :
Proposed Theories
- Metabolic
- Immune
- Vascular
- Infection
- Trauma
- Anatomical and histological anomalies of temporal bone
Genetic :
Autosomal dominant inheritance with incomplete penetrance. Monozygotic twins have 100% concordance rate. Significant association present between both familial and sporadic cases of clinical otosclerosis and COL1A1 gene
Measles Infection :
- Ultrastructural and immunohistochemical evidence of measles like structures and antigenicity in active otosclerotic lesions.
- Measles RNA in footplate specimens with otosclerosis
- Elevated levels of Antimeasles antibodies in perilymph
- Data inconclusive
Clinical Features :
- Conductive or mixed hearing loss
- Slowly progressive
- Bilateral,asymmetric
- Paracusis willisii : Patient hears better in noisy surroundings
- Vestibular symptoms
- Vertigo
- Tinnitus
- Speech : Monotonous,well modulated soft speech
Pathology of Conductive Hearing Loss :
- Fibrous fixation of footplate : 30 db
- Localised bony fixation : 30-40 db
- Bony ankylosis of annular ligament : 40 db
- Impairment of annular ligament at posterior vestibular joint space : 250-2000Hz
Pathology of Sensorineural Hearing Loss :
- Otosclerotic involvement of cochlear endosteum
- Atrophy of spiral ligament and replacement by amorphous eosinophilic substance
- Bony invasion of scala tympani of cochlea
- Circulatory changes in cochlea due to abnormal bone
- Damage to cochlea by metabolic enzymes from abnormal bone
Otomicroscopy :

- Schwartze Sign
- Reddish hue seen through the tynpanic membrane
- Also called flamingo sign
- Indicative of active focus
- Rule out other conditions:
- Middle ear effusions
- Tympanosclerosis
- Tympanic membrane perforations
- cholesteatoma or retraction pockets
Tuning Fork Tests
- Show conductive hearing loss
| MILD | MODERATE | SEVERE | |
| 256 | NEGATIVE | NEGATIVE | NEGATIVE |
| 512 | POSITIVE | NEGATIVE | NEGATIVE |
| 1024 | POSITIVE | POSITIVE | NEGATIVE |
Audiometry :
- Pure tone audiometry
- Impedence audiometry
- Tympanometry
- Acoustic reflex

Pure Tone Audiometry :
Air Conduction
- Low frequencies affected first
- Rising air line-stiffness tilt
- Due to stapes fixation
- Disease progression
- Air line flattens •
- Due to mass effect
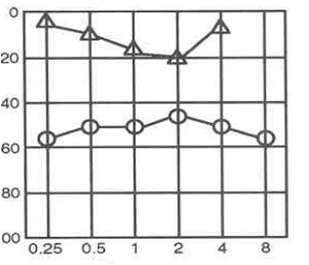
Bone Conduction :
Carhart’s Notch -Hallmark audiologic sign of otosclerosis
Proposed Theory :
- Loss of inertia of stapes
- Fixation disrupts the normal ossicular resonance(2000Hz)
- Normal compressional mode of bone conduction is disrupted because of relative perilymph immobility.
- Reverses with stapes mobilization

Tympanometry :
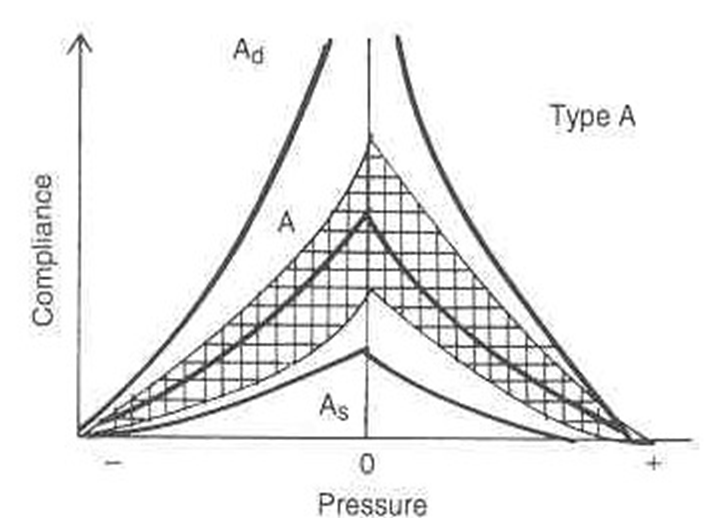
Acoustic Reflex :

Imaging :
Computed tomography(CT) of the temporal bone for evaluation of otosclerosis
Pre-op:
- Characterize the extent of otosclerosis
- Severe or profound mixed hearing loss
- Evaluate for enlarged cochlear aqueduct •
Post-op:
- Recurrent CHL
- Re-obliteration vs prosthesis dislocation
Axial cuts :
- Patient position- canthomeatal line perpendicular to the table top
- 1mm cuts
- Top of superior semicircular canal to bottom of the cochlea •
Coronal :
- Patient position-supine with head overextended face turned 20 degrees ipsilateral
Fenestral Otosclerosis :
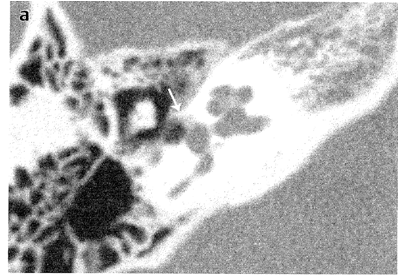
Cochlear Otosclerosis :

Differential Diagnosis :
- Secretory otitis media
- Ossicular discontinuity
- Congenital stapes fixation
- Malleus head fixation
- Tympanosclerosis
- Paget’s disease
- Osteogenesis imperfecta
Treatment Of Otosclerosis
MEDICAL AMPLIFICATION SURGERY
Sodium Flouride
- Mechanism: Flouride ion replaces hydroxyl group in bone forming fluorapatite
- Resistant to resorption
- Increases calcification of new bone •Causes maturation of active foci of otosclerosis
- DOSE – Active lesion-50 to 75mg/day, Maintenance-25mg
Indications of Sodium Flouride
- Surgically confirmed otosclerosis
- Pure SNHL
- Positive radiographic findings
- Positive schwartze sign
- Active focus at surgery-treat for 2 yrs
- Preoperatively
Contraindications of Sodium Flouride
- Chronic nephritis with nitrogen retention where urinary excretion of fluoride may be impaired
- Chronic rheumatoid arthritis
- Pregnant or lactating women
- Children before skeletal growth completed
- Allergy to fluoride
- Skeletal fluorosis
Benefit is demonstrated by:
- Fading of positive schwartze sign
- Stabilization of progressive SNHL
- Reduction of tinnitus
- Improvement of mild vestibular symptoms
- X-ray demonstration of recalcification of the focus
Side Effects -Gastric intolerance, skeletal flurosis
Surgery for Otosclerosis
Indications of Surgery :
- Bone conduction of 0-25dB
- Air conduction of 45-65dB
- Air-bone gap of atleast 15dB
- Speech discrimination of 60% should be present for good hearing improvement
Contraindications :
- Presence of general medical disease
- Old age > 70 yrs
- Conductive losses from other causes
- Presence of otitis externa,tympanic membrane perforation
- Presence of only hearing ear
- Unilateral otosclerosis
- Stapedial and cochlear otosclerosis with poor air-bone gap
- Pregnancy
- Presence of labyrinthine hydrops
- Positive Schwartze sign
- Patients with occupation related to sports,flying aircraft
Informed Consent
- Patient should be informed about amplification as an alternative mode
- Description of the procedure
- Advantages and possible disadvantages of surgery
- Discussion of all potential risks
- Proper counselling for patients with occupations exposing them to significant pressure variations-pilots,divers,parachuters
Anesthesia :
Choice of anesthesia depends on patient’s and surgeon’s preferences .
Local Anaesthesia -Intraoperative reports of vestibular stimulation can be identified
General Anaesthesia– Provides assurance against pain and head movement
Proper Positioning of Patient: Essential for good visualization of middle ear structures •Head of the patient is turned towards the contralateral shoulder •Head tilted downwards 10 to 15 degrees •Use of separate head rest
Canal Wall Injection :

- Infiltration using 1%lidocaine and 1:1,00,000 adrenaline
- Four quadrants of external auditory canal injected
- Infiltration of the canal skin at the level of bony and cartilaginous junction
Elevation of Tympanomeatal Flap
- 6 o’clock to 12 o’clock positions
- 6-8mm lateral to the annulus
- Elevation of flap proceeds anteriorly
- Fibrous annulus displaced from its sulcus
- Posterior half of tympanic membrane folded forwards over handle of malleus
Curettage of Scutum

- Chorda tympani nerve is gently freed from any mucosal folds
- Postero-superior bony annulus removed using bone curette or drill
- To provide exposure of long process of incus,stapes,oval window,facial nerve and base of the pyramid
Middle Ear Exammination :
- Mobility of ossicles
- Confirm stapes fixation
- Evaluate for malleus or incus fixation •Anatomical anomalies
- Dehiscent facial nerve
- Overhanging facial nerve
- Persistent stapedial artery
- Tympanosclerosis
Separation of Incudostapedial Joint
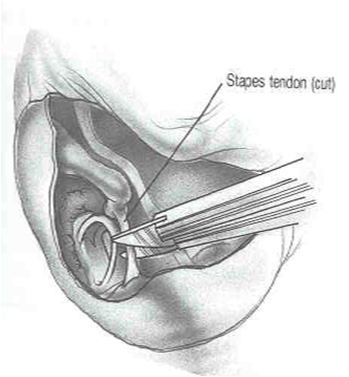
- Stapedial tendon is cut with scissors as close as possible to the pyramidal eminence
- Incudostapedial joint is separated with a joint knife
- Posterior crus is fragmented near its base using crurotomy scissors
- Suprastructure is fractured downward toward promontory and removed from middle ear
- Footplate is transected transversely using sharp angled and straight picks into 2 or 3 pieces
- Gently extracted from the oval window using right angled hooks or microforceps
- Soft tissue graft is used to cover or fill the oval window and prosthesis positioned
- If anterior fragment of footplate is fixed,partial oval window defect covered with soft tissue graft
- Tympanomeatal flap is replaced and the external ear canal packed
Stapedotomy :
- Instrumentation
- Manual/handheld perforator
- Burr with low speed micromotor
- Laser
- Site of fenestration
- Size of fenestration and prosthesis
- Techniques :
- Conventional technique
- Fisch technique
Stapedotomy – Conventional Technique :
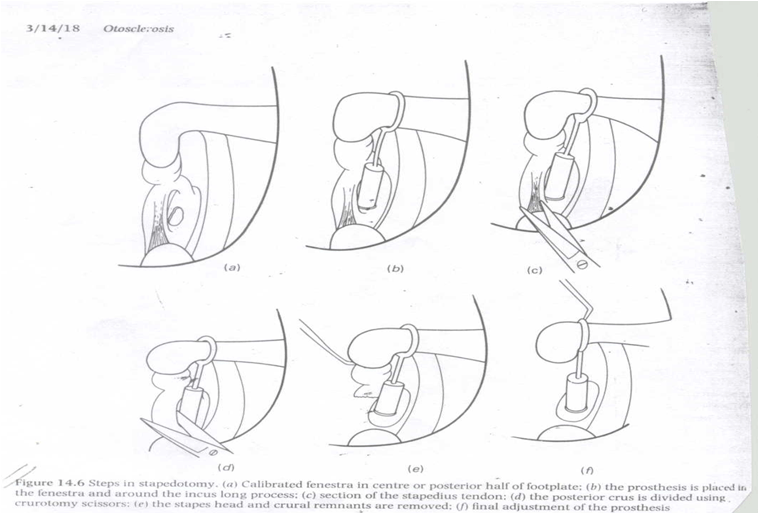
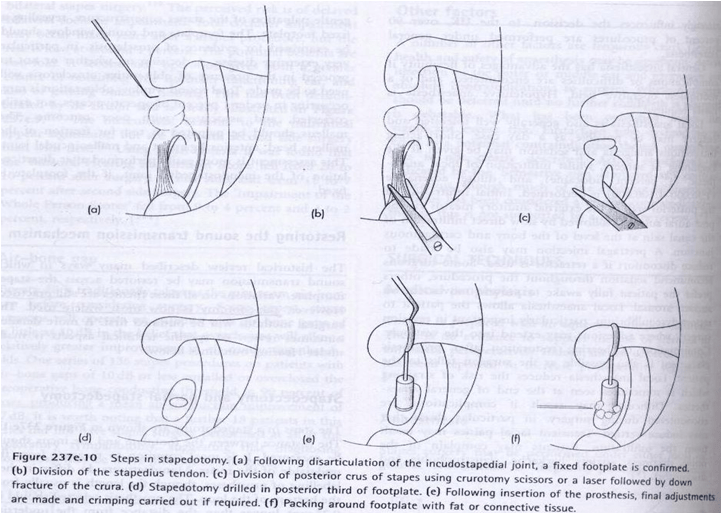
Stapedotomy-Fisch Technique
Stapedectomy v/s Stapedotomy :
- STAPEDECTOMY : •
- Better low frequency hearing gain
- May be only method technically possible
- STAPEDOTOMY :
- Better high frequency hearing gain
- Low incidence of perilymph fistula,SNHL,lateralization of graft
- More stable hearing gain •
- Less labyrinthine trauma
Lasers :
Four important laser qualities for stapedectomy/stapedotomy:
- Precise optics and tissue interaction
- Vapourisation without adjacent thermal spread
- No heating of perilymph
- No penetration of perilymph
Types of Lasers :
- Visible Laser
- short wavelength
- Argon 514nm,KTP 532nm:
- ideal optical properties,effective delivery,visible-working and aiming beam are same
- Infrared Laser
- long wavelength
- Co2 laser: 10,600nm
- Invisible:aiming beam required

Connective Tissue Seal :
- Vein
- Temporalis fascia
- Tragal perichondrium
- Blood clot
- fat

Site of Fenestration :
- Fenestra is placed in the posterior half of the footplate •
- Posterior fenestra– 0.8mm diameter
- Prosthesi– 0.6mm diameter
Reasons for Posterior Fenestra :
- Minimizes the chance of damaging the saccule
- reconstruction of the annular ligament with restoration of proper acoustic impedance
- Adhesions may be present between the saccule and the footplate at the level of the annular ligament anteriorly
- Avoidance of anterior otosclerotic foci reduces the risk of releasing proteolytic enzymes into the inner ear and reduces the chance of bleeding
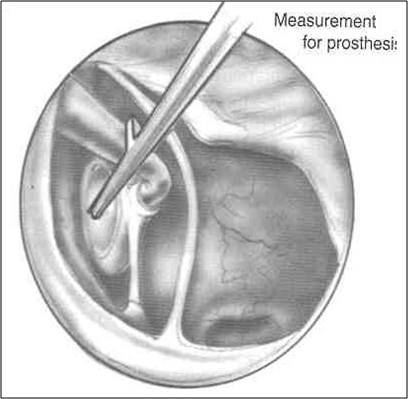
Measurement for Prosthesis :
- Distance between the lateral aspect of long process of incus and footplate should be measured
- Prosthesis selected should be 0.25mm longer than the distance
- Usually ,4.5mm prosthesis will be selected
Types of Prosthesis :
- Robinson prosthesis(metal)-does not require crimping,easy to insert and self centering
- Causse type(teflon)-memory,no crimping
- Fisch/Mcgee -malleable ribbon like crook connected to metal or teflon stem,crimping required
- House type(wire prosthesis)
- Titanium prosthesis
Post Operative Care :
- Keep ears dry
- Avoid strenuous physical activities
- Avoid nose blowing and forceful sneezing
- Avoid air travel
- Oral antibiotics for 1 week
Intraoperative Complications :
- Tears in tympanomeatal flap
- Subluxation of incus
- Overhanging facial nerve
- Obliterative Otosclerosis of oval window
- Otosclerosis involving the round window
- Persistent stapedial Artery
- Malleus Ankylosis
- Perilymph gusher
- Floating Footplate
Postoperative Complications :
- Facial palsy
- Chorda tympani dysfunction
- Otitis media
- Vertigo
- Reparative Granuloma
- Sensorineural Hearing loss
- Conductive Hearing loss
Tears in Tympanomeatal Flap :
- REASONS:
- Elevation of the flap in a limited segment,not in a broad front
- Elevation of tympanic membrane without the annulus
- REPAIR:
- Placement of a medially placed tragal perichondrium or fascia graft
- Small tears-closed with piece of gelfoam
- Small linear tears-Avoid infolding of the edges of the tear
Subluxation of Incus :
- Reasons:
- During curettage of the bony annulus
- Separation of the incudostapedial joint
- Manipulation around oval window
- During crimping
- Treatment
- Incus attachment prosthesis
- Malleus attachment prosthesis

Overhanging Facial Nerve :
- If the prolapsed nerve abuts the promontory inferior to the oval window,surgery should not be completed
- Surgery can be completed by drilling a small fenestra that includes the inferior aspect of the annular ligament
- Prosthesis must be longer than usual to accomodate bending inferiorly to avoid the nerve
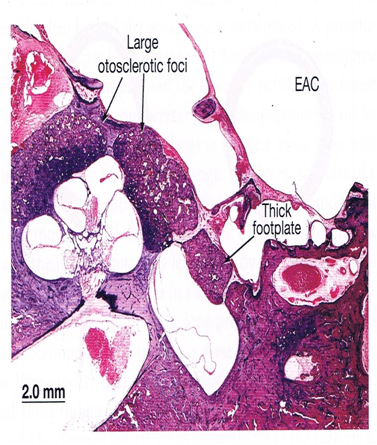
Obliterative Otosclerosis of Oval Window :
- Oval window niche can be obliterated by severe thickening of the stapedial footplate or margins of niche
- Fenestration can be achieved after first saucerizing the obliterated niche and thinning the obstructing bone
- If obliterative otosclerosis is found in one ear, 50% chance of the same finding to be present in other ear
Otosclerosis Involving the Round Window :
- Round window can be partially or completely obliterated by otosclerosis
- Surgery should be completed and the finding noted in the operative note
- residual conductive loss is present following surgery,revision surgery is not recommended
Persistent Stapedial Artery :

- Arises from the internal carotid artery, often seen running across the footplate
- Incidence: 1 in 5000 to 10,000 ears
- Cannot be safely coagulated with bipolar cautery or laser
- Often it occupies only the anterior half of the footplate and fenestration can be completed in the posterior half
Malleus Anklosis :
- Head of malleus ankylosed to the roof of epitympanum by a spur or bar of bone
- Etiology not associated with that of otosclerosis
- Incidence of malleus fixation: 0.5%
- Unilateral in contrast to otosclerosis
- Fixation of the malleus can be corrected by removing the incus and head of malleus and reconstruction with a malleus attachment prosthesis
Perilymphatic Gusher :
- Associated with patent cochlear aqueduct
- More common on the left
- Increased incidence with congenital stapes fixation
- Increased risk of SNHL
Management :
- Rapid placement of the soft tissue seal over oval window,then the prosthesis
- Elevation of head end
- Bed rest
- Avoid valsalva
Floating Footplate :
- Footplate dislodges from the surrounding OW niche
- More commonly iatrogenic
- Prevention
- Use of laser
- Preliminary footplate control hole
- Management
- Abort and place soft tissue
- Small drill hole at margin of oval window and hook to remove
Perilymphatic Fistula :
- Most common single complication of stapedectomy:9-10%
- Potentially dangerous risk of meningitis,hearing loss and dysequilibrium
Etiology :
Primary Fistula :
Presesnt at end of surgery •Syrgeon creates and relies on healing process •Fistula common with plastic prosthesis •Small fistula becomes large with barotraumas •
Secondary Fistula :
Appears many months or years after surgery-usually due to barotraumas Common when stapedial tendon is cut
Diagnosis :
Symptoms :
- Dysequilibrium
- Hearing loss
- Tinnitus
- Fluctuating hearing •
Audiometric Tests :
- PTA- Sensorineural loss in low frequency
- Speech discrimination- initially fluctuates,later reduced
Treatment :
- Tympanotomy •
- Excision of tract,removal of prosthesis,covering the defect by soft tissue
Facial Nerve Injury :
- Temporary injury
- Immediate facial nerve palsy postoperatively due to local anaesthetic infiltration
- Delayed facial palsy between days 4 and 10 postoperatively
- Due to facial nerve swelling,resulting from the nerve being heated by a drill or laser
- Permanant injury
- rare
- Associated with laser or burr injury in the presence of a dehiscent canal
Chorda Tympani Dysfunction :
- Damage to chorda tympani nerve is seen in 30% of procedures
- Sectioning or stretching the nerve leads to:
- Metallic taste
- Impairment of taste
- Dry mouth
- soreness of tongue
- Stretching produces more symptoms than sectioning
Post operative Vertigo :
- Serous labyrinthitis – 1week post op
- Reparative granuloma
- Depressed footplate
- Bony fragments compressing the saccule
- Suppurative labyrinthitis
- Endolymphatic hydrops
Post opretive conduction Hearing Loss :
- Displacement or dislodgement of the prosthesis from oval window area(36%)
- Necrosis of long process of incus
- Loose attachment between incus and prosthesis
- Detachment of prosthesis from incus
- Recurrence of otosclerosis and oval window closure
Post Operative Sensorineural Hearing Loss :
- Incidence-0.6%
- Temporary-serous labyrinyhitis
- Permanent
- Surgical trauma
- Sudden release of perilymph pressure
- Excessive movement of stapes
- Rupture of membranes of inner ear
- Vascular compromise
Reparative Granuloma :
- Granulation tissue formation around the prosthesis and incus
- 1-2 weeks postop
- Initial good hearing results followed hearing loss
- Associated tinnitus and vertigo
- O/E: Dull and reddish discolouration of tympanic membrane in postero-superior quadrant
- Treatment: Immediate exploration and removal of granulation tissue
- Prognosis: Hearing returns with early excision